Breast Implant Reconstruction After Mastectomy: “Ask Amy”
A couple of weeks ago I asked you what questions YOU had for me.
I wanted to know what the biggest challenge is in your life when it comes to your body right now.
And I got some really interesting submissions that I'm looking forward to sharing with you!
I already took the time to answer each person directly but I'm going to choose one topic and it answer it for everyone here today.
Whether or not this specific question applies to you, I hope you might be able to learn something from the thought process behind I how I answer because so often this is where the true answers lie.
BREAST IMPLANT RECONSTRUCTION AFTER MASTECTOMY: Is it right for you?
The decision whether or not to reconstruct breast mounds after a mastectomy is a very personal one.
Mastectomy changes your body forever and, for many women, this is not only physically challenging but mentally and emotionally difficult as well.
The most common choice after mastectomy is some form of breast mound reconstruction instead of wearing artificial prosthetics, typically with breast implants.
We are lucky that newer options are becoming more widely available and recognized, such as aesthetic flat closure and advances in natural tissue transfer (DIEP, tram, lat, and other flap surgeries).
But for many, breast implants are still the most straight forward path to a desired or familiar shape after breast cancer and mastectomy.
So how do you know if it's right for you or not?
Let's go through some of my client's questions (and a few more) to see if we can find the answer.
Implants can be a straight forward path to a desired or familiar shape after breast cancer and mastectomy.
HER QUESTION: Are implants worth the extra surgery?
This might be the fundamental question when it comes to any reconstruction option.
Surgery is hard and mastectomy recovery often includes drains that are irritating and difficult to manage.
The pain and loss of sensation (often followed by HYPER sensation as nerves fire up again) is unfamiliar to most of us and the idea of going through this again on purpose can be daunting.
But for many, many women the benefits of rebuilding breast mounds outweighs the cons of surgeries.
One way to help you determine if implants are “worth” additional surgery is to understand what these surgeries may look like so let's dig deeper.
For many women the benefits of rebuilding breast mounds outweighs the cons of surgeries.
How many actual surgeries are involved with implants?
Like almost everything in cancer land, the not so simple answer is “it depends”.
In my career I have seen everything from ONE to FIFTEEN with 3-5 being the most common answer.
There are many factors that determine how many surgeries you might end up having if you opt for implant reconstruction.
what your surgeons discover about your tumor size and placement during surgery or through additional pathology
whether or not radiation therapy is part of your treatment plan
what size your natural breasts are and what size implant you are looking for
will you be having your implants placed under the pectoralis major muscles (UTM) or on top (OTM also called pre-pectoral)
are you eligible for “direct to implant” which negates the need for tissue expanders
if you experience any complications such as infection or rejection
do you require/desire fat grafting or other revisions to improve your results
the preference of your breast and/or plastic surgeons
I was very lucky in that I am one of the few I know who only had ONE surgery with my mastectomy and reconstruction.
On May 22, 2017 I underwent a 7 and ½ hour surgery where they:
removed both my breasts in a bilateral mastectomy
placed my permanent silicone implants in a “direct to implant” pre-pectoral surgery
removed my ovaries and fallopian tubes (bilateral salpingo-oopherectomy or BSO)
Some of the factors that determined this outcome were:
the size and location of my tumor (small and away from the chest wall)
the size of my breasts vs. my desired size after implant (comparable)
the integrity of my skin and tissue after mastectomy (healthy)
I did not need radiation as part of my treatment plan
I was satisfied with my results and chose not to have any revisions
Going into surgery I was told I had a 5% chance of the direct to implant option so I fully anticipated waking up with expanders which would have required at least one additional surgery down the road.
MOST people end up with AT LEAST two surgeries:
mastectomy and placement of expander
exchange of expander for permanent implant
But it is not uncommon AT ALL to also end up with:
Skin sparing mastectomy with or without expanders
a complication requiring a removal and replacement of an expander
if both breasts are involved sometimes they are not done at the same time
implant exchange
revision surgeries by choice or necessity
The best thing you can do if you are considering implant reconstruction and how many surgeries YOU might require is to talk to your team about these various factors and ask them how many surgeries they believe you will need (barring complications or anything unexpected).
Once you have this information you may also want to consider:
that every surgery has risks and increases the possibility of complications
how well you personally tend to recover from anesthesia and surgery
your tolerance for pain, discomfort, and downtime
your lifestyle and how surgery will impact that (family, work, activities)
And then… is there another surgery on the horizon?
Surgeries associated with implant reconstruction range but average 3-5 with revisions.
HER QUESTION: Is it true they need to be changed every ten years or so?
Implants have come along way over the last few decades.
Silicone implants are now considered as safe as saline and much more durable and effective in creating a satisfactory shape.
Regardless of which style you choose it is important to monitor not only the health of your body but the health and integrity of your implants while they are in your body.
Depending on your unique needs and/or the preference of your plastic surgeon you may have imaging, like breast MRI, to make sure all is well with the structure and placement of your implants.
While it used to be common to replace them on a ten year timeline, it is more common now to look at you and your implants on an individual basis.
Before deciding on implant reconstruction talk to your doctors about how they approach this question.
My own surgeon told me that as long as my implants are in good shape and I am still happy with them they may remain as they are for up to 20 years or more!
And, I know from personal experience, that these guys can take a beating.
Only 5 months after surgery, while still in active chemo, I tripped walking down the street and flew through the air like superman to LAND FACE DOWN ON MY CHEST WITH MY ARMS OUT IN FRONT OF ME.
I spent the next morning barely able to breathe (pretty sure I bruised a few ribs) and googling "how much pressure/impact can silicone implants take, but when I had my screening MRI a couple of years later (because upon physical examination my surgeon was not concerned) they were in perfect form.
At this point I have no intention to replace my implants unless there is a problem that requires it or I am told it is simply necessary for my best interest.
Yay science!
So while this is my story and experience, again it will always come back to YOU and YOURS.
Monitoring the health and integrity of your implants is an important part of the process.
HER QUESTION: How long after a mastectomy, do you feel sort of normal?
This is such a complex question and truly I don't have proven statistics or simple facts to draw on for this so I'm going to share my personal response to her:
"I don't believe there is a finish line of recovery that we all get to cross and be like oh good here is my new normal!
Barring any complications, I would say for most people "normalcy" (or maybe it's more adjusting to the new way you are now) comes within about a year or two, but I've seen people find acceptance and comfort in their bodies much sooner and also take a lot longer.
My own experience with mastectomy and implant reconstruction definitely took a while to adjust, especially because I had chemotherapy afterwards, but I would say by a year out from surgery I was getting used to the daily feel of my new breasts.
There are many contributing factors that can play into how long your recovery and adaptation takes but I do think that after a while our brains start to forget the way things USED to be and begin to recognize the way they are, hence some form of new normalcy."
Now a few final thoughts…
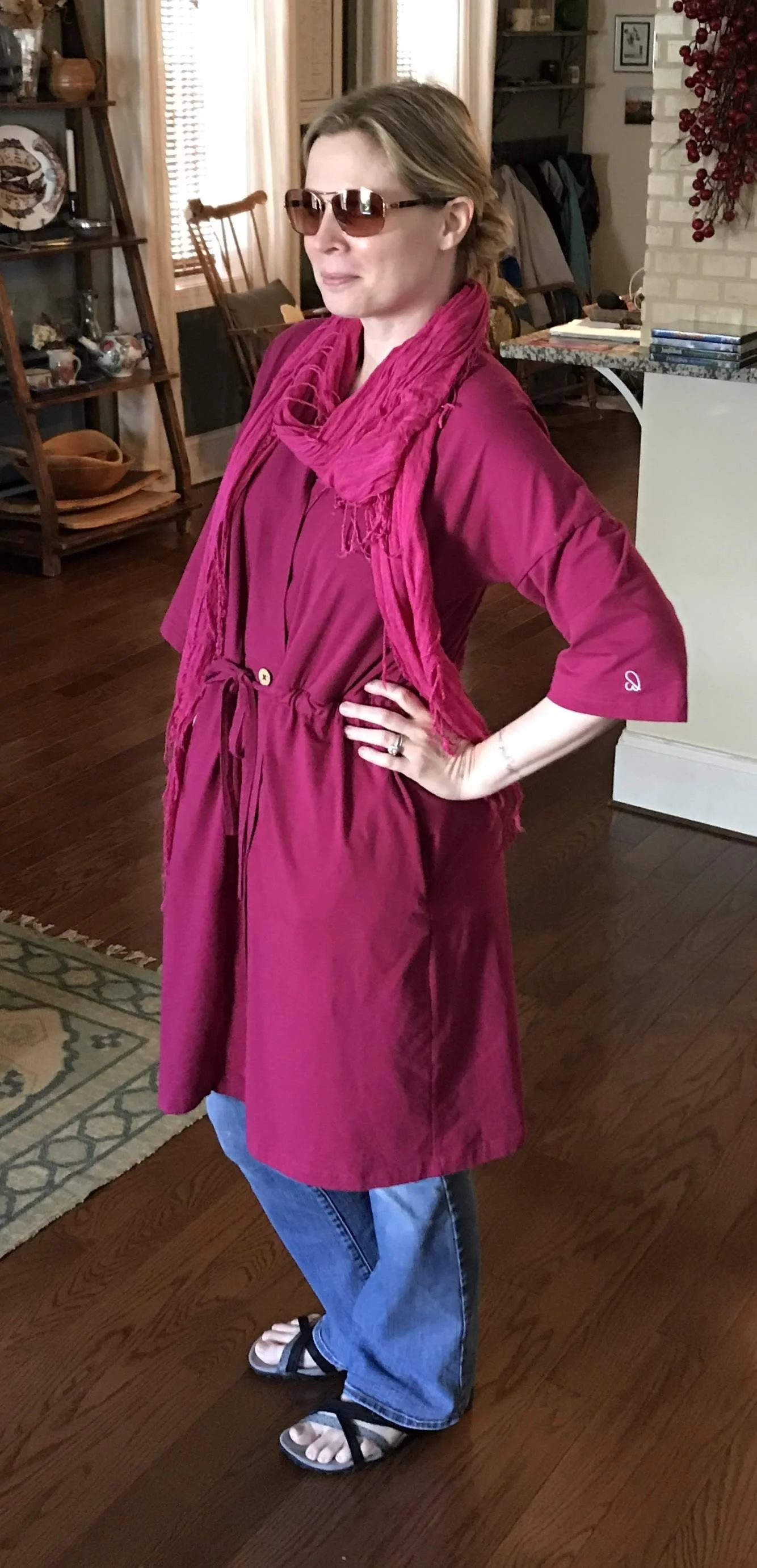
Dressed and posing in my “drain robe” about a week after my surgery. I was a long way from “normal”.
I'm guessing you can see by this newsletter that there are no simple answers to any of these questions but there are ways to find YOUR answers.
The most important thing you can do for yourself is to get educated and informed on your body, your diagnosis, and your options.
This remains true in recovery and survivorship as well!
Only you can decide if something like implant reconstruction is worth it for you, so I will finish by saying that given my personal experience, for me it has been.
So I would love to know - if you had implant reconstruction - has it been worth it???
Want more free content? Sign up for the The Sunday Self-Care Chronicles and get weekly insight and inspiration from the intersection of personal and professional experience in breast cancer land sent directly to your inbox.