Traveling After a Breast Cancer Diagnosis - Part 2: On the Move ✈️ 🚉 🚙
DISCLAIMER: All information in this article is for educational and informational purposes only. It is not intended as medical advice or treatment. Always consult your healthcare team before beginning any new self-care activity or practice.
Traveling in modern times has many conveniences and also a lot of headaches.
An itinerary including planes, trains, automobiles can translate to long lines, frustrating delays, lost luggage, and cancelled hotel rooms.
The last thing you need whether traveling for work or pleasure is the added discomfort of a lymphedema flare up or pain from scar tissue and limited range of motion.
In Part 1 of this series, “Planning and Packing”, I looked at things you can do in advance of your trip to help make things easier and more enjoyable when traveling after a breast cancer diagnosis.
Now it’s time to dive into the travel itself!
Luggage Management
As a seasoned traveler I love challenging myself to see how much I can stuff into the smallest luggage possible. However on longer trips, even with laundry facilities along the way, a carry-on alone is just not realistic.
Whether you are wheeling your largest suitcase or stuffing a duffel in the overhead bin, luggage is something to give a little extra consideration to when you’ve had a breast cancer diagnosis.
One reason is that almost everyone who has gone through breast cancer has some level of risk for secondary lymphedema, a chronic condition that can result in painful swelling.
Not familiar with breast cancer-related lymphedema? READ THIS NOW.
Lymphedema Risk
What does your favorite AWAY bag have to do with lymphedema?
The quick answer is that common breast cancer interventions like lymph node biopsy, removal, and radiation therapy can damage lymph nodes and vessels creating a risk of developing the condition.
While the mechanics behind it are a bit more complicated, over-stressing an area of the body that is at risk - like the shoulder, arm, and hand in the case of breast cancer - can lead to aggravation, inflammation, and potentially, a lymphedema flare up.
So, when you are lifting that heavy suitcase that just squeaked under the 50lb weight limit, or balancing your expanded carry-on over your head, or even loading that packed cooler in and out of the trunk of your car, you might be doing more than your body is used to or ready for.
Scar Tissue and Surgical Recovery
The same things that can be said of lymphedema risk can also apply to recent surgery or radiation. Even if your weight restrictions have been lifted following a procedure that doesn’t mean your body may be ready for a lot of heavy lifting or reaching.
Pay attention to your current range of motion and work within it whenever possible. Even years out you might find that the affected side of your body doesn’t have the same strength or stamina as the rest of you.
Chemo/Immune/Hormone Therapies and Fatigue
Anyone who’s been through the “red devil” or takes tamoxifen or an aromatase inhibitor knows the lasting affects of joint pain and fatigue.
Additionally, hormone suppression or forced menopause can create a risk of osteopenia or osteoporosis making bones more fragile than they might otherwise be.
Luggage may be a necessary part of traveling but approach it with common sense so that you can enjoy your trip instead of bringing more pain home as a souvenir or wearing yourself out before you even get there.
Here are things I try to be mindful of when it comes to my luggage, no matter the means of transportation:
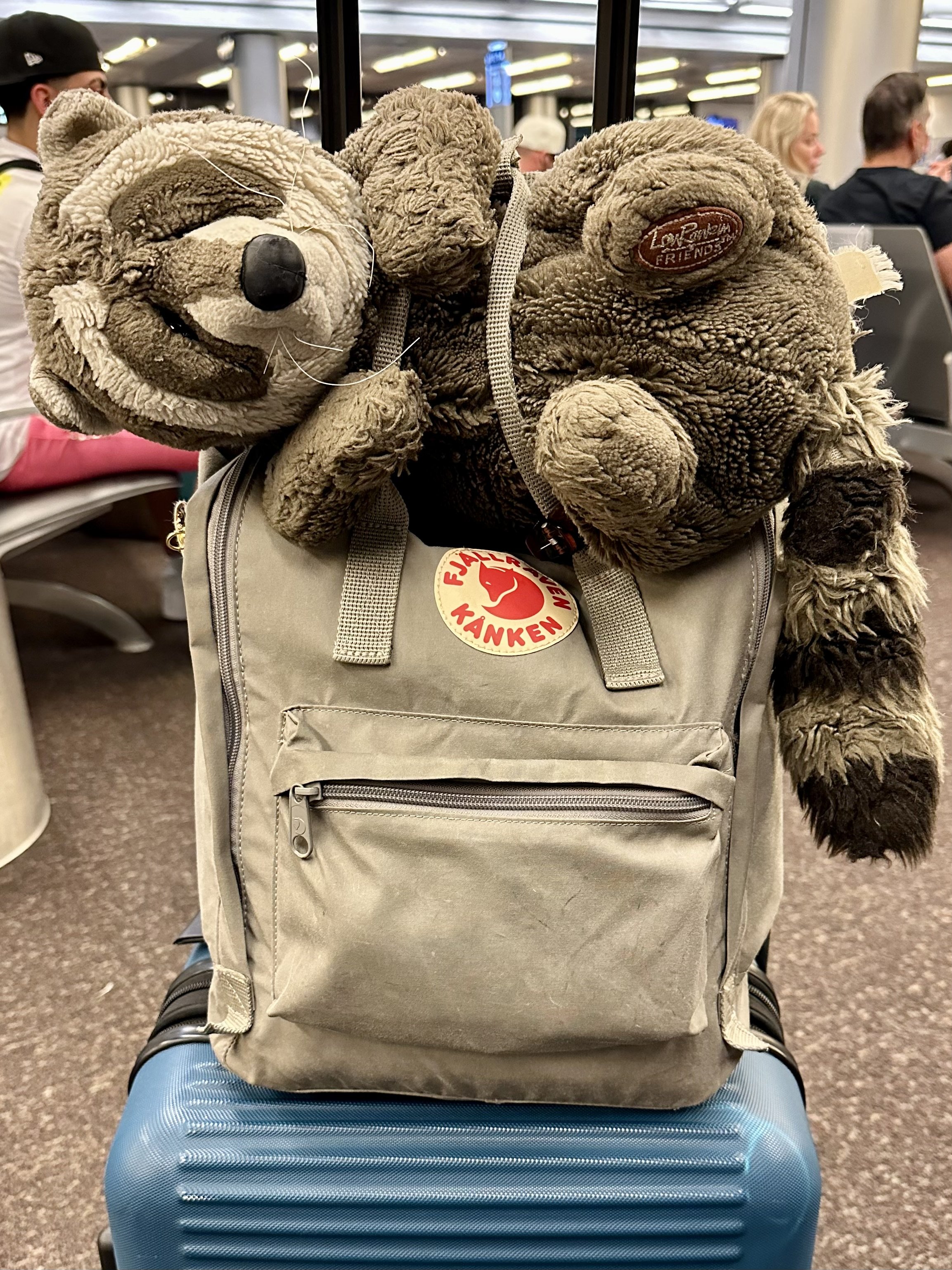
Let the wheels do the work. Whenever possible I find wheeling bags to be the way to go. Even my carry-ons have wheels or at least a strap so I can stack them on my wheeled bag. And if I have to resort to carrying something on my shoulder then I make sure it’s a backpack and I use BOTH straps to balance things evenly.
Let your “other side” bear the load. We all have a dominant hand or arm that tends to be our go to especially for lifting heavy objects. If this also happens to be your “cancer side” then try using your other hand for the heavier luggage.
Make multiple trips. Traveling is not a strong man competition. There is no prize for how much you can lift at once. This is often more applicable if you are traveling by car and may have more to load in and out but this is definitely a case where less is more.
Know your body and its limitations. If you are someone who lifts heavy objects or weights on a regular basis then hoisting up your luggage may not be a big deal. But if this is not your regular routine, or you’re still early in your healing, then try to limit how much you are lifting and how high.
When in doubt ask for help! I have never been in a situation where some kind person - whether a flight or train attendant or another passenger - wasn’t willing to help me when I asked. A sincere thank you goes a long way and they will feel good for having lent a hand.
Even my favorite travel companion gets strapped in for the ride when I’m wheeling luggage around the airport!
On the Go - In the Air or On the Ground
Flying - Short Flights
Shorter flights are less likely to present problems when it comes to lymphedema risk* but I personally feel more confident when I wear a compression sleeve no matter how the long flight is.
If you don’t have a sleeve you can ask your doctor or lymphedema therapist for a Rx for one to have on hand.
I put my sleeve on an hour or two before my flight (or last minute if I completely forget!) and then leave it on for about the same amount of time after I land.
Also, while ginger ale and salty peanuts are my favorite in-flight snack for a quick trip I always make sure to grab at least one cup of water each time they pass by to help balance my body’s fluid load.
*if you have an actual lymphedema diagnosis I always recommend wearing a properly fitted sleeve when flying regardless of distance.
Flying - Long Hauls
Overnight flights are great if you are able to sleep but we all know what it’s like to be cramped in the middle seat for any length of time.
In addition to compression sleeves, extra movement becomes super important for every 60 minutes you add to your flying time.
There are a few things that you can do right in your seat like shoulder and wrist rolls, side to side rotation from your waist, and of course don’t forget to bend your knees and ankles.
I also try to reach my arms and hands up above my head frequently (just pretend you’re adjusting the fan or light but don’t accidentally hit the call button!) to get circulation moving.
On really long flights, when everyone is else is sleeping, I’ve even been known to get up and do some easy stretches and yoga poses to get my blood and lymph moving. There’s nothing like a narrow aisle between rows to practice your Warrior 2 alignment (but whatever you do please don’t try Child’s Pose on the cabin floor - straight yuck)!
Trains
While not quite as common in the U.S., train travel is accessible and ample throughout many parts of the world, especially Europe.
While some of the same logic applies as logging air time, you may not have to bother with a compression sleeve (unless it’s already part of your routine or you wear it to support lifting all that luggage).
And the great thing about many trains is that you have free rein to get up and wander from car to car. Just finding the bathroom or bar car can be enough time to give your legs a good stretch and relieve stiff joints.
Automobiles
While often the easiest way to travel, especially locally, long car rides still need to be thought through.
Consider planning out bathroom breaks and using them for at least a five minute stretch and to check your supplies.
Keep snacks and plenty of water in the car so that if you end up on a highway with no rest stops in sight you can keep on keeping on.
Security & TSA
Depending on your mode of transportation and destination your passport might not be the only documentation you need to bring along.
Prescription & OTC Medications
While it’s not required to have your prescription medications in their original bottle, if you are on regular medications like tamoxifen or an aromatase inhibitor (Letrozole, Anastrozole, Exemestane) or any type of important Rx that shouldn’t be skipped, it doesn’t hurt to have proof of pills with you in case you get questioned.
Medical Device Cards
If you have any sort of implanted medical device that may set off a metal detector or other security imaging machine it’s important to have documentation with you.
Most devices have a card that you are given (even implants have these!) and having this on hand can save you a lot of unwanted hassle or potentially embarrassment.
Pre-Check or Extra Assistance
Consider enrolling in TSA Pre-Check or other Trusted Traveler programs if you travel frequently. Not only will it save time but it usually limits the amount of hassle you need to deal with at the airport or train station.
One of the best things my husband and I ever did was enroll in Nexxus which works for border states in North America. We are able to zip through the land border into Canada since we fly out of Toronto for most of our international flights and, when flying domestically, I can leave my shoes and belt on and all of my electronics in my bag! All for $50 every 5 years.
With or without any kind of pre-check arrangement you can also ask for special assistance or screening procedures to get you through security with less stress.
Traveling with Company vs. Alone
If you were not a seasoned traveler BEFORE your breast cancer diagnosis but you are now looking to make the most of life consider beginning your adventurous way in the company of others.
Family, friends, or even a group tour can be great ways to receive a little extra support and assistance when on the go.
Talk to them in advance about what you may need and keep them updated along the way to reduce frustration or miscommunication. More than likely the WANT to support you and help you enjoy your trip!
And if you are traveling on your own, allow yourself to be a bit honest and vulnerable, and open up when appropriate.
When people ask me about my sleeve I tell them why I wear it - I had breast cancer and I’m at risk of lymphedema and this helps me reduce that risk.
If I need to ask for help with heavy luggage or multiple bags, I’m not afraid to throw the cancer card out there as an explanation so they know I’m not just being lazy or weak (and so what if I was, I get by with a little help from my friends… and strangers!).
This guy has been around the world with me! His only downfall is he can’t help me with my luggage.
In Summary (TL:DR):
Luggage:
Pack as light as possible when possible.
Use wheeled or balanced luggage like a backpack to ease your load.
Be very mindful lifting and reaching with heavy bags and when in doubt ask for help!
On the Go:
Wear a compression sleeve when flying if appropriate for your diagnosis or risk. Not sure what’s right for you? Ask your local Certified Lymphedema Therapist or book an “Ask Amy” Consultation with me and let’s talk it through!
Make sure to move your body even in your seat. Stretch your limbs and get up and walk around as much as possible during long trips of any kind.
Stay hydrated and nourished. Dehydration can increase risk of fluid imbalance and worsen a lymphedema diagnosis or cause a flare up.
Security:
Have any necessary medical or device documentation with you to make screenings easier.
Consider a pre-check program to help reduce hassle or ask for special assistance.
Traveling Alone:
Try to travel with company if you aren’t familiar with traveling alone since your diagnosis (or at all).
Be willing to be honest and ask for help from staff and fellow strangers when needed.
Even the actual traveling part doesn’t have to be something you endure.
I have learned to love the journey and not just the destination, it just takes a little forethought and planning, to make it safe, easy, and enjoyable.
In Part 3 we’ll be talking about the best part - your destination and time away! - so stay tuned!
I hope this post has been helpful!
Any questions? Comment below or shoot me a DM on Instagram and don’t forget to check out my previous posts here on The Sunday Self-Care Chronicles!
Amy Hartl is a Board Certified, NYS Licensed, Oncology Massage & Certified Manual Lymphatic Drainage Therapist specializing in Breast Cancer.
Growing up BRCA1+ meant breast cancer was part of Amy's life even before her actual diagnosis. She first turned her prophecy into a career in 2012 to help others but, after a double mastectomy, chemotherapy, and surgical menopause in 2017, she now uses her knowledge and skills to continue healing herself too.
When not elbow-deep in entrepreneurship or advocacy at home in Buffalo, NY, she loves traveling the world with her husband, family, and friends.
She likes to thank her cancer diagnosis and Lexapro for curing her lifelong fear of flying because she’s since been to the other side of the world, flown in tiny planes (and loved it!), and even gone paragliding in the Swiss Alps.
She is a Gen-X Swiftie with a long standing love for Buffy the Vampire Slayer, Kenny Rogers, tattoos, and overalls.
And while Amy may never think of breast cancer as a gift, she does know that she is stronger because of it and lives life more fully in the face of it.
NOTE: The Sunday Self-Care Chronicles and all content written for Amy Hartl, LMT and As We Are Now LLC is written from my perspective as a cis-gendered white woman. Because this is my lived experience and what I know and can speak to, and because MOST people diagnosed with breast cancer are assigned female at birth (AFAB), I often use terms like “she, her, woman, etc..” However I recognize that breast cancer does not discriminate by race, by gender assignment or expression, or any other label or identifier that we use in our society. Therefore, this space, my free content, and my online services are all available to you, whoever you are, if you are living with a breast cancer experience.
I am also well aware that many people who are diagnosed with breast cancer will never see an end to treatment. For those still living with breast cancer, especially metastatic breast cancer, life “after” or “beyond” breast cancer may refer to diagnosis vs. an end to treatment but I use this language interchangeably and invite you to apply it how you will to your personal experience.
Want to receive The Sunday Self-Care Chronicles directly to your inbox every week?